For Consultation:
Spinal Tumors
A spinal tumor is an abnormal mass of tissue within or surrounding the spinal cord and spinal column, in which cells grow and multiply uncontrollably, seemingly unchecked by the mechanisms that control normal cells. Spinal tumors can be benign (non-cancerous) or malignant (cancerous). Primary tumors originate in the spine or spinal cord and metastatic or secondary tumors result from cancer spreading from another site to the spine.
Spinal tumors may be referred to by the area of the spine in which they occur. These basic areas are cervical, thoracic, lumbar and sacrum. Additionally, they are also classified by their location in the spine – anterior (front) and posterior (back). Clinically, they are divided according to location into three major groups: intradural-extramedullary, intramedullary, and extradural.
1) Intradural-extramedullary: These tumors develop in the spinal cord's arachnoid membrane (meningiomas), in the nerve roots that extend out from the spinal cord (schwannomas and neurofibromas) or at the spinal cord base (filum terminale ependymomas). Although meningiomas are often benign, they can be difficult to remove and may recur. Nerve root tumors are also generally benign, although neurofibromas may become malignant over time. Ependymomas at the end of the spinal cord can be large, and treatment may be complicated by the delicate nature of fine neural structures in that area.
2) Intramedullary: These tumors grow inside the spinal cord or individual nerves, most frequently occurring in the cervical (neck) region. They typically derive from glial or ependymal cells that are found throughout the interstitium of the cord. Astrocytomas and ependymomas are the two most common types. They are often benign, but can be difficult to remove. Intramedullary lipomas are rare congenital tumors most commonly located in the thoracic spinal cord.
3) Extradural: These lesions are typically attributed to metastatic cancer or schwannomas derived from the cells covering the nerve roots. Occasionally, an extradural tumor extends through the intervertebral foramina, lying partially within and partially outside of the spinal canal.
• Metastatic spinal tumors -
The spinal column is the most common site for bone metastasis. Estimates indicate that at least 30 percent and as high as 70 percent of patients with cancer will experience spread of cancer to their spine. Common primary cancers that spread to the spine are lung, breast, and prostate. Lung cancer is the most common cancer to metastasize to the bone in men, and breast cancer is the most common in women. Other cancers that spread to the spine include gastrointestinal tract, lymphoma, melanoma, kidney, sarcoma, and thyroid.
Prompt diagnosis and identification of the primary malignancy is crucial to overall treatment. Numerous factors can affect outcome, including the nature of the primary cancer, the number of lesions, the presence of distant nonskeletal metastases, and the presence and/or severity of spinal cord compression.
• Pediatric spinal tumors -
Primary spinal tumors are rare in children and challenging to treat. Incidence and outcome vary by histological subtype, which is quite broad. These include osteoid osteoma, osteoblastoma, osteochondroma, osteosarcoma, Ewing sarcoma, eosinophilic granuloma, aneurysmal bone cyst, chordoma, mesenchymal chondrosarcoma, giant cell tumor of bone, fibrous dysplasia, fibroma, angiosarcoma, and hemangioma. Unlike adults, children have not achieved complete skeletal growth, which must be taken into account when considering treatment. Other things to consider are spinal stability, surgical versus nonsurgical interventions, and preservation of neurological function.
• Incidence and Prevalence -
Intracranial (brain) tumors account for 85 to 90 percent of all primary central nervous system (CNS) tumors. Primary tumors arising from the spinal cord, spinal nerve roots, and dura are rare compared to CNS tumors that arise in the brain. Overall prevalence is estimated at one spinal tumor for every four intracranial lesions. About 10,000 Americans develop primary or metastatic spinal cord tumors each year.
Intramedullary tumors are rare, accounting for only 5 to 10 percent of all spinal tumors. Benign tumors such as meningiomas and neurofibromas account for 55 to 65 percent of all primary spinal tumors.
Meningiomas most frequently occur in women between the ages of 40 and 70.
Metastatic spinal tumors are the most common type of malignant lesions of the spine, accounting for an estimated 70 percent of all spinal tumors.
1) Causes:
The cause of most primary spinal tumors is unknown. Some of them may be attributed to exposure to cancer-causing agents. Spinal cord lymphomas, which are cancers that affect lymphocytes, a type of immune cell, are more common in people with compromised immune systems. There appears to be a higher incidence of spinal tumors in particular families, so there is most likely a genetic component. In a small number of cases, primary tumors may result from presence of these two genetic diseases:
• Neurofibromatosis 2: In this hereditary disorder, benign tumors may develop in the arachnoid layer of the spinal cord or in the supporting glial cells. However, the more common tumors associated with this disorder affect the nerves related to hearing and can inevitably lead to loss of hearing in one or both ears.
• Von Hippel-Lindau disease: This rare, multisystem disorder is associated with benign blood vessel tumors (hemangioblastomas) in the brain, retina and spinal cord and with other types of tumors in the kidneys or adrenal glands.
2) Symptoms:
Non-mechanical back pain, especially in the middle or lower back, is the most frequent symptom of both benign and malignant spinal tumors. This back pain is not specifically attributed to injury, stress or physical activity. However, the pain may increase with activity and is often worse at night. Pain may spread beyond the back to the hips, legs, feet or arms and may worsen over time, even when treated by conservative, nonsurgical methods that can often help alleviate back pain attributed to mechanical causes.
Depending on the location and type of tumor, other signs and symptoms can develop, especially as a malignant tumor grows and compresses on the spinal cord, the nerve roots, blood vessels or bones of the spine. Impingement of the tumor on the spinal cord can be life-threatening in itself. Additional symptoms can include:
• Loss of sensation or muscle weakness, in the legs, arms or chest
• Difficulty walking, which may cause falls
• Decreased sensitivity to pain, heat and cold
• Loss of bowel or bladder function
• Paralysis that may occur in varying degrees and in different parts of the body, depending on which nerves are compressed
• Scoliosis or other spinal deformity resulting from a large but benign tumor
3) Diagnosis:
A thorough medical examination with emphasis on back pain and neurological deficits is the first step. Radiological tests are required for an accurate and positive diagnosis.
• X-ray: Application of radiation to produce a film or picture of a part of the body can show the structure of the vertebrae and the outline of the joints. X-rays of the spine are obtained to search for other potential causes of pain, i.e. tumors, infections, fractures, etc. X-rays are not very reliable in diagnosing tumors.
• Computed tomography scan (CT or CAT scan): A diagnostic image created after a computer reads x-rays; can show the shape and size of the spinal canal, its contents, and the structures around it. Very good at visualizing bony structures.
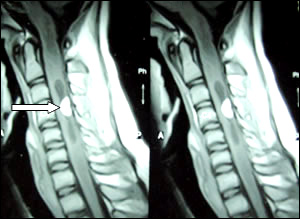
• Magnetic resonance imaging (MRI): A diagnostic test that produces three-dimensional images of body structures using powerful magnets and computer technology; can show the spinal cord, nerve roots, and surrounding areas, as well as enlargement, degeneration, and tumors.
After radiological confirmation of the tumor, the only way to determine whether the tumor is benign or malignant is to examine a small tissue sample (biopsy) under a microscope. If the tumor is malignant, biopsy also helps determine the cancer's type, which provides information that helps determine treatment options.
Staging classifies neoplasms (abnormal tissue) according to the extent of the tumor, assessing bony, soft tissue, and spinal canal involvement. A whole body scan utilizing nuclear technology may be ordered, as well as a CT scan of the lungs and abdomen for staging purposes. The above findings and results from laboratory tests are compared to the patient's symptoms to confirm diagnosis.
• Nonsurgical treatment -
Nonsurgical treatment options include observation, chemotherapy, and radiation therapy. Tumors that are asymptomatic or mildly symptomatic and do not appear to be changing/progressing, may be observed and monitored with regular MRIs. Some tumors respond well to chemotherapy and others to radiation therapy. However, there are specific types of metastatic tumors that are inherently radioresistant (i.e. gastrointestinal tract and kidney), and in those cases, surgery may be the only viable treatment option.
1) Surgery:
Indications for surgery vary depending on the type of tumor. Primary spinal tumors may be removed through complete en bloc resection for a possible cure. In patients with metastatic tumors, treatment is primarily palliative, with the goal of restoring or preserving neurological function, stabilizing the spine, and alleviating pain. Generally, surgery is only considered as an option for patients with metastases when they are expected to live 12 weeks or longer and the tumor is resistant to radiation or chemotherapy. Indications for surgery include intractable pain, spinal cord compression, and the need for stabilization of impending pathological fractures.
In cases in which surgical resection is possible, preoperative embolization may be used to enable an easier resection. This procedure involves the insertion of a catheter or tube, through an artery in the groin. The catheter is guided up through the blood vessels to the site of the tumor, where it delivers a liquid embolic agent similar to glue, which blocks the vessels that feed the tumor. When the blood vessels that feed the tumor are blocked off, bleeding can often be controlled better during surgery, helping to decrease some of the risks.
The posterior approach allows for the identification of the dura and exposure of the nerve roots. Multiple levels can be decompressed epidurally, and a posterior multilevel segmental fixation can be performed. The anterior approach is excellent for decompressing ventral tumors and effectively reconstructing the anterior column. This approach also allows placement of short-segment fixation devices. Thoracic and lumbar spinal tumors that affect both the anterior and posterior vertebral columns are a challenge to resect completely. Traditionally, a posterior (back) approach followed by a separately staged anterior (front) approach has been utilized surgically to treat these complex lesions.
2) Recovery:
The typical hospital stay after surgery to remove a spinal tumor is about 5-10 days, depending on the patient’s case. A period of physical rehabilitation is required post surgery, which may require a stay in a physical rehabilitation hospital for a period of time. In other cases, physical therapy may take place at an outpatient facility or at the patient’s home. The total recovery time after surgery may be as short as three months or as long as one year, depending on the complexity of the surgery and the patient’s overall health.
3) Outcome:
Outcome depends greatly on whether the spinal tumor is benign or malignant, primary or metastatic, and on the age and overall health of the patient. In the case of primary tumors, the goal is to remove the tumor completely, leading optimally to potential cure of the malignancy. In the case of metastatic tumors, the goal is almost always palliative. At best, treatment may provide the patient with an improved quality of life and prolonged life expectancy.
Contact Details
Mobile: +91 98308 34566
Email:
pbishnu04@yahoo.co.in
pbishnu08@gmail.com
Website:
www.neurosurgeryindia.co.in